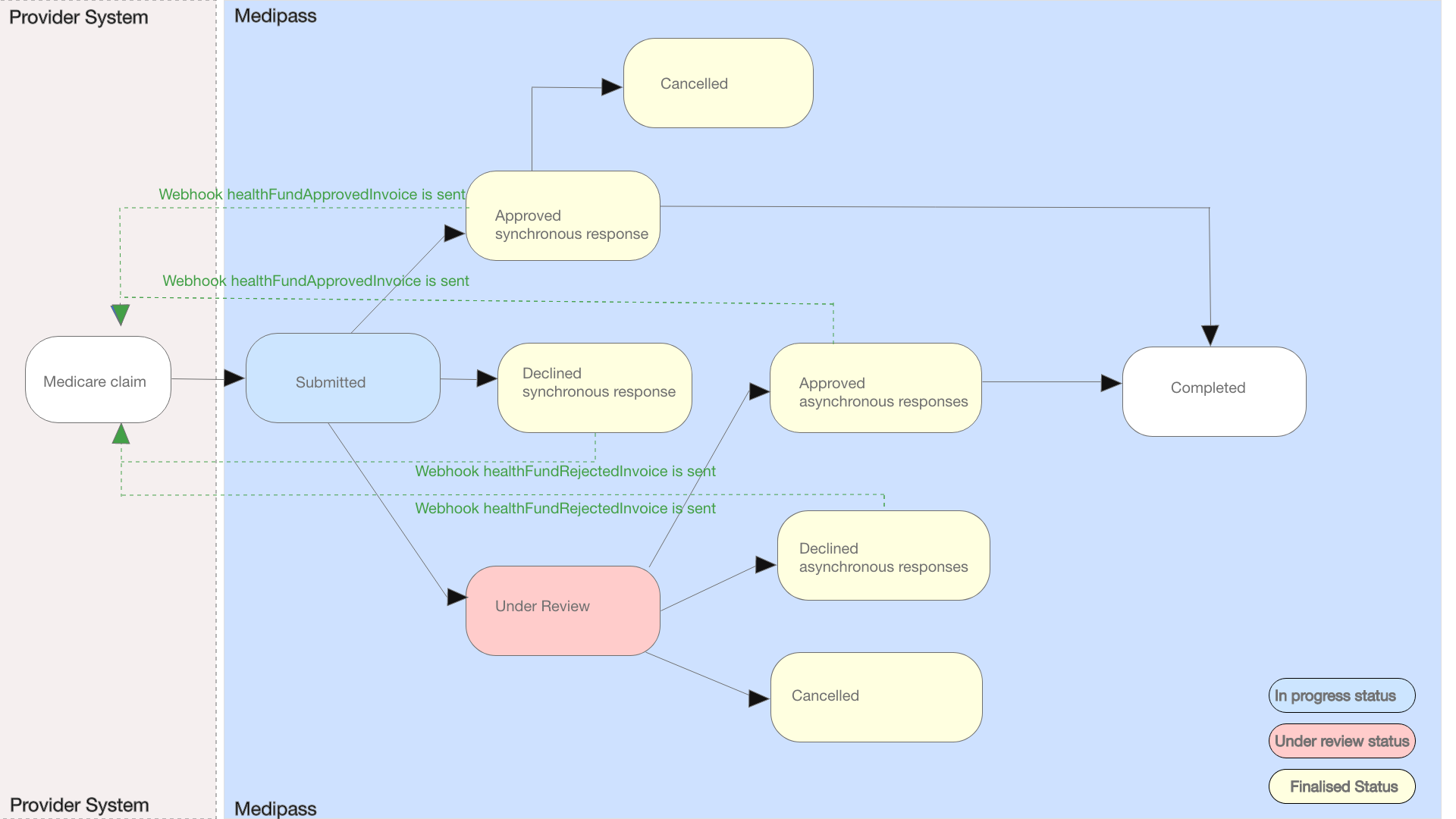
Medicare claims- also called invoices - will have both synchronous and asynchronous outcomes. Patient claims are adjudicated in real-time with a synchronous response provided within 15 seconds. Bulk billed claims are asynchronous, with adjudication responses ranging from hours to typically two business days from submission. Partners will need to accommodate for asynchronous responses which can be pushed from Tyro Health via webhooks or periodically polled by partners via an invoice status API.
Once a claim is submitted, the status can change as follows:
Outstanding : claim is under review by MedicareApproved : claim is approved for settlementDeclined : claim was declined and will not be paidCancelled : claim was canceled by the provider prior to settlementCompleted : approved claim paid/settled to provider
If multiple service items are claimed and one item is rejected the whole invoice will be marked as Declined.
Approved Medicare Patient Claims are settled by Services Australia to the claimant's nominated bank account. Approved Medicare Bulk Bill Claims are settled by Services Australia to the service providers nominated bank account.
To issue a successful claim, the following details are required in each invoice:
- Provider, profession and location : Usually set with a single provider number attribute. These details must be registered with Tyro Health in advance of a claim. Only one provider can claim per invoice.
- Patient Details: including first and last name, date of birth,card number,individual reference
- Service items: including date of service, item number and fees are required. Optional attributes can include service text , accession date,number of patients seen SPI ID, collection time and other item attributes. Multiple service items from multiple service dates can be claimed per invoice.
Medicare does not currently support attachments however Invoice level service text is supported. If an attachment is required to support a claim those details must be sent directly to Medicare by the provider.
Medicare currently support electronic claims from:
- Aboriginal and Torres Strait Islander Health Practice
- Acupuncture
- Ambulance
- Audiology
- Chinese Medicine
- Chiropractic
- Counselling
- Dental
- Diagnostic Imaging
- Dietetics
- Exercise Physiology
- General Health Equipment
- General Practice
- Genetic Counselling
- Home Care service and Aids
- Hospital
- Mental Health
- Myotherapy
- Naturopathy
- Nursing and Midwifery
- Occupational Therapy
- Optometry
- Orthoptics
- Orthotics/Prosthetics
- Osteopathy
- Pathology
- Perfusion (Medical)
- Pharmacy
- Physiotherapy
- Podiatry
- Psychology
- Radiology
- Remedial Massage
- Social Work
- Specialist Physician
- Specialist Treatment centres
- Speech Pathology
Medicare is a nationwide insurance scheme with eligible patients in all states and territories. Providers in all states and territories are welcomed to join and enable Medicare claiming.
Providers must first register with Tyro Health prior to submitting a Medicare claim. This registration process is self-service and can be completed within a few minutes. If providers deliver services from multiple locations or businesses, each unique provider number must be registered. Details on provider registration and Medicare activation is provided at:https://help.medipass.com.au/en/articles/4064976-activating-medicare-and-dva-claiming-in-medipass
Any eligible medicare member with a valid medicare card can use this service.
To be eligible for Medicare benefits patients have to fall under one of the following categories:
- an Australian or New Zealand citizen
- an Australian permanent resident
- a patient who has applied for permanent residency (some conditions apply)
- a patient who is a temporary resident covered by a Ministerial Order
- a patient who is a citizen or permanent resident of Norfolk Island, Cocos Islands, Christmas Island or Lord Howe Island
- a patient who is covered by a Reciprocal Health Care Agreement with another country
For more details on who is eligible for Medicare please see: https://www.servicesaustralia.gov.au/enrolling-medicare?context=60092#whocan
Patients can have more than one active claim with Medicare at the same time.
The Medicare integration does not currently support patient quotes for services to be rendered. Tyro Health plans to introduce these capabilities in a future update. Tyro Health provides a verification service that can be used to check Medicare patient details and Concession eligibility in advance of a claim. This resource provides a more seamless claiming experience for your patients on day of service and can be used to determine potential to claim benefits.
The service will verify multiple attributes of a Medicare account, including:
- First name
- Last name
- Date of birth
- Medicare card number
- Medicare individual reference
- Medicare account status
- Sex
- Concession status
For claiming and account verification, Providers need to be registered with Medicare and hold an active Medicare issued provider number at each servicing practice to be enabled for online claiming. Providers must also lodge an application form, even if previously registered for online claiming. This application covers both Medicare and DVA claiming registration. Tyro Health Online provides an assisted account setup and activation process to complete and lodge these forms: https://help.medipass.com.au/en/articles/3193875-signing-up-for-medipass.
Providers can lodge Medicare claims 24/7.
Most claims are processed instantly by Medicare using their straight-through adjudication method. Those claims will return an approved or declined status within 15 seconds and the SDK will return that status via a callback.
Claims that cannot be instantly processed will require manual review by Medicare case managers. Other claims which contain miscellaneous, general catch-all and special items will also go into under review status for manual review when submitted.
Invoices that are placed Under Review at the time of submission will be handled manually by a Medicare claims manager. This typically occurs during business hours Monday-Friday.
Once the provider's invoice has been approved by Medicare within Tyro Health, funds will be deposited to your nominated bank account the following business day by Tyro Health.
Tyro Health automatically generates patient reports, statements and receipts on behalf of the partner/providers. These reports and receipts can be obtained from the Tyro Health Online provider portal or via API calls.
Invoices are automatically generated by Tyro Health Online for each employee and the treatments delivered. These invoices are directly sent to Medicare's for approval. Providers can print copies of the invoice from the Tyro Health Online provider portal or invoice details can be generated by a partner PMS for print or email to patients.
Remittance reports are available on the Tyro Health Online when the payment has been made. Remittance reports will include all payments to a provider for the given settlement period which can include payments for other funding sources such as icare, Medicare and payment cards.